Melanoma Patient Story
With over ten years of experience as a facial plastic and reconstructive head & neck surgeon on the MedStar Skin Cancer Team, I have seen too often how seriously skin cancer can affect people’s lives. I would like to share the story of Susanne, a lovely patient of mine, who has a long history of squamous cell carcinoma (SCC) and recently underwent successful treatment for melanoma of the right cheek. Susanne regularly visits her dermatologist and had noticed a concerning spot on her face. In January 2022, her dermatologist performed a biopsy, which revealed melanoma, measuring 1.1 mm thick. Based on the biopsy results, Susanne’s dermatologist referred her to our Multidisciplinary Skin Cancer Team based at Medstar Georgetown University Hospital. Our team quickly scheduled her for an evaluation.
Susanne was reasonably concerned given melanoma’s reputation as the most dangerous skin cancer due to its ability to spread to other parts of the body; even though she had fought several other skin cancers in the past, the melanoma diagnosis felt different and was scary. She mentioned she realized the magnitude of the situation when she saw how quickly we booked her for surgery.
During our pre-operative visit, we discussed Susanne’s diagnosis and plan for treatment. I did my best to answer all of her questions in plain English. When asked what made her comfortable proceeding with this procedure, Susanne said, “Dr. Reilly was very knowledgeable but made everything understandable. You could tell he knew what he was doing but he also wasn’t speaking Greek. He explained what the scar would look like and the results were very accurate.” She also said, “I talked to my nurse practitioner and told her what was going to happen and mentioned Dr. Reilly and she said I absolutely had the ‘A-team’. Before my tele-visit I was quite nervous, but after meeting Dr. Reilly, I kept thinking ’everything is going to be fine’.”
Susanne’s right cheek melanoma was 1.1 mm deep, which warranted a margin of more than 1 cm of normal skin be removed around all sides of the lesion. This left a wound measuring 3.5 x 5.0 cm (about 1.4 x 2.0 inches) after removal. The depth of Suzanne’s melanoma also warranted a sentinel node biopsy. In a sentinel lymph node biopsy, a nuclear medicine specialist will inject a radioactive tracer into the area of skin surrounding the melanoma. They then use a nuclear scan to acquire images that determine which lymph nodes are responsible for draining the area of the skin lesion. Following the scan, the patient is brought to the operating suite, where I then inject a blue dye called Isosulfan Blue into the skin around the skin lesion. The combination of the visual cue of the blue dye and the auditory signal from the radioactive tracer helps me to locate the affected lymph node(s), which I then remove. I order to repair a 1.4 x 2.0 inch defect of the cheek with matching skin color and contour, I performed a cervicofacial rotation flap. This procedures involves elevating the skin from the adjacent face and neck and essentially stretching it in a uniform fashion in order to cover the wound. When tissue is rotated like this, there is most often the need to create additional “releasing” incisions on either side of the flap to prevent puckering of the skin or “pincushioning” at the point of rotation.
Susanne had a successful and speedy recovery; she admits that the scars were a little scary at first, but of all the procedures she has had under anesthesia, this recovery was the easiest. She did not have any bandages on her face, which is a difficult area to keep a dressing on. Instead, the incisions on her face and neck were covered regularly with petroleum jelly, which is considered an “occlusive” dressing since it is impermeable to bacteria and/or water. Within a week or two Susanne was stunned by her progress. She noted that even her friends were shocked to find out how fast she recovered. Below is a series of photographs showing the recovery process at different points in time.
Melanoma can be a scary diagnosis to get. Surgery on the face can be anxiety-provoking, especially when it is as extensive as what is required for effectively treating melanoma. It is essential for patients to find a provider who is experienced in the treatment of both melanoma and the the reconstruction following removal of a melanoma. As a double board-certified Head & Neck Surgeon and Facial Plastic & Reconstructive Surgery, I am grateful that so many patients like Susanne entrust me with their care in these difficult times and honored to be part of their care.
SENSITIVE CONTENT WARNING: The following photos contain sensitive content which some people may find offensive or disturbing.
Waking up in the recovery room:
Two days after surgery:
Nine days after surgery:
Eleven days after surgery:
Twenty-two days after surgery:
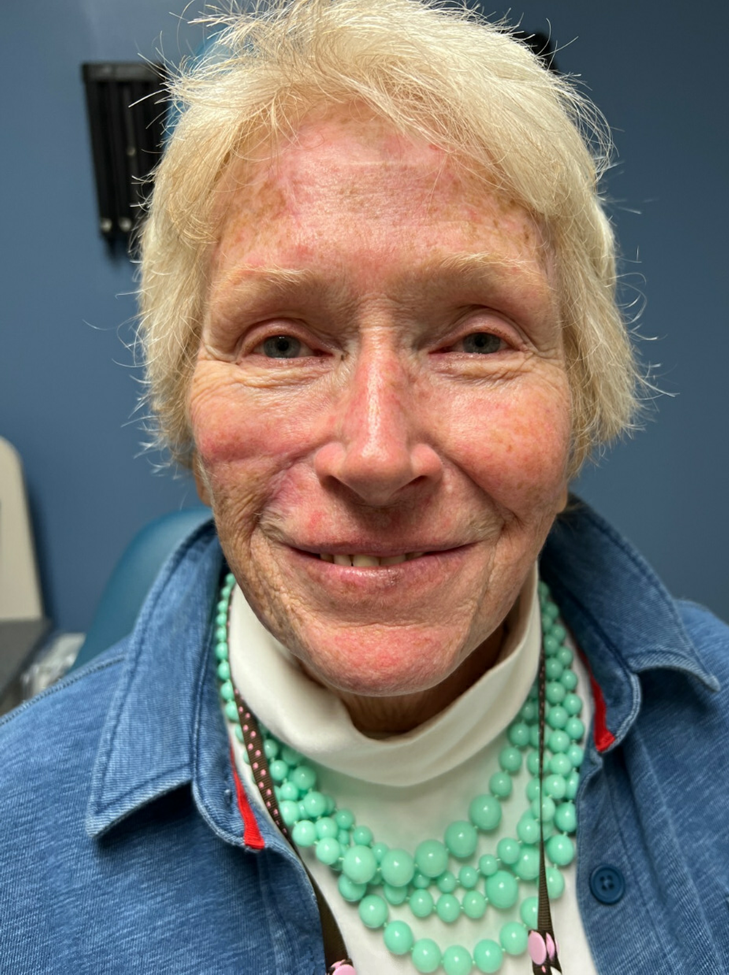
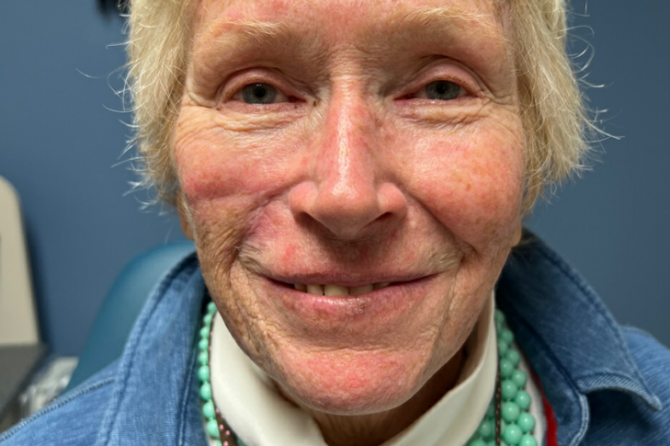
Three months after surgery:
Leave a reply